EMS providers should be familiar with key aspects of asthma and associated respiratory emergencies. Here are some important points to consider:
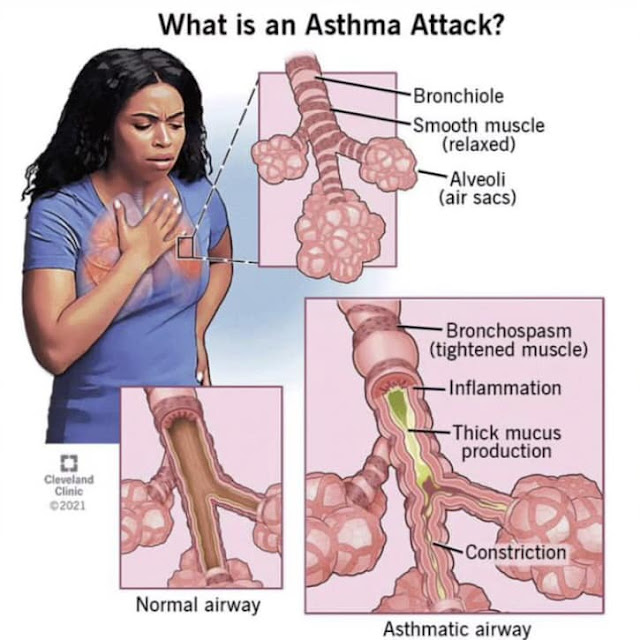
Asthma Overview: Understand that asthma is a chronic inflammatory condition of the airways, characterized by recurrent episodes of wheezing, coughing, chest tightness, and shortness of breath. It can range from mild to severe, and triggers may include allergens, exercise, respiratory infections, or environmental factors.
Signs and Symptoms: Recognize the signs and symptoms of an asthma attack, such as audible wheezing, increased respiratory rate, use of accessory muscles, coughing, cyanosis (bluish discoloration), and difficulty speaking in full sentences.
Assessment: Perform a thorough respiratory assessment, including checking the patient's oxygen saturation levels, lung sounds, and respiratory effort. Assess the severity of the asthma attack using a validated scoring system, such as the Asthma Severity Score.
Treatment: Administer high-flow supplemental oxygen to maintain adequate oxygenation. Consider providing bronchodilator medications, such as albuterol, through a nebulizer or metered-dose inhaler with a spacer. Corticosteroids may also be administered to reduce airway inflammation.
Monitoring: Continuously monitor the patient's vital signs, oxygen saturation, and respiratory status. Reassess the patient's response to treatment periodically and adjust interventions accordingly.
Complications: Be aware of potential complications, including respiratory failure, pneumothorax (collapsed lung), and status asthmaticus (severe, prolonged asthma attack refractory to treatment). Promptly recognize and manage these complications as needed.
Communication: Communicate effectively with the patient and their caregivers, providing reassurance and explaining the actions being taken. Obtain a thorough medical history, including any known asthma triggers or previous exacerbations.
Transport and Referral: Determine the appropriate level of care and transport the patient to the nearest appropriate healthcare facility. Ensure a smooth handoff to the receiving medical team, providing them with a detailed report of the patient's condition, interventions performed, and response to treatment.
Remember, asthma management should be individualized based on the patient's condition and medical history.
Regular training, updated protocols, and close coordination with medical direction are crucial for providing optimal care to patients experiencing asthma and associated respiratory emergencies.
#Asthma #ChronicInflammatoryDisorder #RespiratoryDistress #RespiratoryFailure
#Cyanosis #Bronchospasm #StatusAsthmaticus